Every year, over 300,000 patients in England acquire airborne viruses while receiving medical treatment in hospitals. This alarming statistic highlights a critical issue within healthcare facilities, where the very environments designed to promote healing can become breeding grounds for infections. In high-income countries, the World Health Organization has reported that 7.6% of patients acquire healthcare-associated infections (HCAIs). In England alone, recent studies indicate that more than 650,000 patients a year are affected, costing the NHS over £1 billion annually. Airborne transmission is responsible for up to 10% of all HCAIs, underscoring the urgent need to address this issue. A multifaceted approach that encompasses technology, policy, and awareness is essential for safeguarding patient health.
The Problem: Understanding Airborne Viruses in Hospitals
Airborne viruses, including influenza, COVID-19, and various respiratory pathogens, pose a significant threat to patient safety within hospital environments. Several factors contribute to the rapid transmission of these viruses, making it essential to understand the underlying issues.
One of the primary challenges is high patient volume. Hospitals frequently operate at or near full capacity, resulting in crowded waiting areas and shared treatment spaces. This congestion increases the likelihood of airborne transmission as patients, caregivers, and healthcare workers share close quarters. In such conditions, the chances of inhaling pathogens from others in the vicinity rise dramatically.
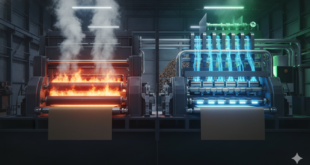
Another critical factor is inadequate ventilation. Many hospital facilities, especially older ones, are equipped with ineffective ventilation systems that fail to filter and purify the air adequately. This lack of proper airflow allows airborne pathogens to linger in the environment for extended periods, significantly heightening the risk of infection among patients and staff alike. A well-ventilated space is crucial in mitigating the spread of viruses, yet many hospitals struggle to meet this basic requirement.
The inconsistent use of personal protective equipment (PPE) further complicates the situation. While healthcare workers receive training on proper PPE usage, adherence to protocols can be inconsistent. This lapse increases the likelihood of accidental exposures to airborne pathogens. Patients with weakened immune systems are particularly vulnerable, making it imperative that protective measures are consistently implemented to safeguard their health.
Finally, the presence of infectious patients in shared spaces presents a considerable risk for airborne virus transmission. When patients with contagious illnesses are treated in common areas—such as emergency departments and waiting rooms—the potential for spreading airborne viruses increases significantly. This scenario creates an environment where healthy individuals can unknowingly be exposed to pathogens, exacerbating the challenges of infection control within hospitals.
Addressing these issues is critical for safeguarding patient health and enhancing the overall safety of healthcare environments. Understanding the dynamics of airborne virus transmission can pave the way for effective interventions and innovative solutions in hospital design and operation.
Solutions: Enhancing Patient Safety and Reducing Infections
To effectively combat the problem of airborne viruses in hospitals, a multifaceted approach is necessary, incorporating technological advancements, policy changes, and educational initiatives. These solutions aim to enhance patient safety and significantly reduce the risk of airborne infections.
Improved Air Quality Management is a fundamental strategy. Hospitals should invest in advanced ventilation systems equipped with high-efficiency particulate air (HEPA) filters, which are proven to effectively capture airborne viruses and other pathogens. By significantly improving indoor air quality, these systems create a safer environment for both patients and staff. Additionally, regular maintenance and monitoring of ventilation systems are essential to ensure their optimal performance, guaranteeing that the air quality remains consistently high.
Another critical solution is the establishment of isolation protocols for infectious patients. Implementing strict protocols for isolating patients known or suspected to carry airborne viruses is crucial in minimizing exposure to others. Designating specific areas with controlled access for these patients can significantly reduce the risk of transmission, protecting both vulnerable patients and healthcare staff from potential infection.
Enhanced personal protective equipment (PPE) is also vital for safeguarding healthcare providers against airborne pathogens. Equipping staff with appropriate PPE, such as N95 respirators, ensures a higher level of protection. Regular training and refresher courses on PPE usage and safety protocols are essential to reinforce adherence among healthcare workers, further mitigating the risk of infection.
Increased awareness and education play a pivotal role in combating airborne viruses. Education campaigns targeting healthcare staff and patients can raise awareness about the risks associated with these pathogens. Informing patients about the importance of hand hygiene and the use of masks can empower them to take proactive steps in reducing transmission.
The expansion of telehealth services has gained momentum, especially following the COVID-19 pandemic. By offering virtual consultations for non-urgent medical issues, hospitals can decrease the number of patients physically present in healthcare settings. This reduction in patient density not only minimizes the risk of airborne virus transmission but also enhances overall patient care.
Finally, regular monitoring and reporting of hospital-acquired infections are crucial for identifying trends and assessing the effectiveness of implemented measures. Establishing a robust system for tracking infection rates can guide future interventions and inform policy changes, ensuring that hospitals remain proactive in safeguarding patient health.
By integrating these strategies, hospitals can create safer environments that not only enhance patient safety but also significantly reduce the risk of airborne infections, ultimately leading to improved healthcare outcomes.
Conclusion: A Collaborative Approach
Addressing the issue of airborne viruses in hospitals requires collaboration among healthcare professionals, facility managers, and policymakers. By prioritizing air quality management, reinforcing infection control protocols, and fostering a culture of awareness and education, hospitals can significantly reduce the risk of airborne virus transmission. Innovative projects like PASTA illustrate the potential for cutting-edge technology to enhance patient safety. Protecting the health and safety of patients must remain a top priority, ensuring that the hospital environment is a place of healing, not infection.
 International Defense Security & Technology Your trusted Source for News, Research and Analysis
International Defense Security & Technology Your trusted Source for News, Research and Analysis