In recent weeks, concern over the emergence of a novel coronavirus in China has grown exponentially as media, experts and government officials around the world have openly worried that this new disease has the potential to develop into a global pandemic. As the ongoing coronavirus outbreak centered in China has spread to other countries and been blamed for a growing number of deaths, a consensus has emerged that this particular virus, currently classified as a “novel [i.e. new] coronavirus,” is believed to have originated in bats and was transmitted to humans in Wuhan, China via a seafood market that also traded exotic animals. So-called “wet” markets, like the one in Wuhan, were previously blamed for past deadly coronavirus outbreaks in China, such as the 2003 outbreak of Severe Acute Respiratory Syndrome (SARS). Viruses that have caused past pandemics typically originated from animal influenza viruses. Zoonotic disease outbreaks occur when a virus, bacterium, or fungus jumps from an animal to a human.
Pandemics put millions of lives are at risk and their economic consequences can run into billions. The 1918 pandemic killed approximately 50 million people around the globe, making it one of the deadliest events in human history. Last Ebola outbreak cost more than 11,000 human lives and more than $32 billion in economic ripple effects while Zika has cost the economies of Latin America and the Caribbean an estimated $18 billion. Eliminating pandemic outbreaks and mitigating the impact of a potential high threat biological agent release are national security priorities.
Pandemics also affect militaries. Warfighters must also operate in regions where diseases like chikungunya and dengue are endemic, and even seemingly mild challenges like seasonal influenza affect force readiness. Military service members are called upon to operate virtually anywhere in the world, often on short notice, and the locations to which they deploy frequently lack the robust public health infrastructure to identify and contain the spread of new viral infectious diseases. Viruses that have caused past pandemics typically originated from animal influenza viruses. Zoonotic disease outbreaks occur when a virus, bacterium, or fungus jumps from an animal to a human.
Maintaining active disease surveillance around the world is costly and time-consuming, accurate prediction of when and where these infections will occur next can enable us to better mitigate these outbreaks before they become epidemics. On January 2018, the Defense Advanced Research Projects Agency (“DARPA”) issued a new solicitation in the form of a broad agency announcement for the Preventing Emerging Pathogenic Threats—or “PREEMPT”—program. PREEMPT, seeks to support military readiness by going after new viral infectious diseases at the source, animal reservoirs—the species in which a pathogen lives, multiplies, and potentially evolves into a strain that can threaten humans. PREEMPT aims to advance understanding of viruses and their interaction with animals, insects, and humans, and deliver new, proactive interventions to reduce the risk from emerging and reemerging pathogens.
In February 2019 , the Defense Advanced Research Projects Agency announced an agreement with scientists at the University of California-Davis, the University of Idaho, and Plymouth University in England to work on the agency’s Preventing Emerging Pathogenic Threats program. DARPA has committed up to $9.37 million in support for the program over 3 1/2 years. The program will be managed by the DARPA Biological Technologies Office, which generally supports activities that integrate biology, engineering, computer science, physical sciences, and mathematics.
Media outlets have also linked the coronavirus outbreak to Biowarfare programs. Several media outlets have promoted claims that the reported epicenter of the outbreak in Wuhan, China was also the site of laboratories allegedly linked to a Chinese government biowarfare program. Earler some media reports expressed the fear that bats could be used as biological weapons, particularly in spreading coronaviruses and other deadly diseases.
Like much of the Pentagon’s controversial research programs, the bats as bioweapons research has been framed as defensive, despite the fact that no imminent threat involving bat-propagated bioweapons has been acknowledged. However, independent scientists have recently accused the Pentagon, particularly its research arm DARPA, of claiming to be engaged in research it says is “defensive” but is actually “offensive.” The Washington Post asserted that the Pentagon’s interest in investigating the potential use of bats to spread weaponized and deadly diseases was because of alleged Russian efforts to do the same.
In addition, while both DARPA’s PREEMPT program and the Pentagon’s open interest in bats as bioweapons were announced in 2018, the U.S. military — specifically the Department of Defense’s Cooperative Threat Reduction Program — began funding research involving bats and deadly pathogens, including the coronaviruses MERS and SARS, a year prior in 2017. One of those studies focused on “Bat-Borne Zoonotic Disease Emergence in Western Asia” and involved the Lugar Center in Georgia, identified by former Georgian government officials, the Russian government and independent, investigative journalist Dilyana Gaytandzhieva as a covert U.S. bioweapons lab.
Zoonotic Viruses
Animals host a massive number of viruses, and sometimes these viruses make the jump to humans. (These viruses are called zoonoses.) That’s because there are a lot of hurdles that an animal virus has to clear before it spreads to a person, and from there, to another person. “A virus doesn’t just jump out of a bat and cause an epidemic in humans,” says Ronald Rosenberg, an infectious disease researcher. Instead, a virus can spend decades or even centuries hopping back and forth between animals and humans before the conditions come together for an outbreak. (The exception are influenza viruses, which can make this leap more rapidly, Rosenberg says. )
Some Researchers are concentrating on humans, once a virus has made that rare leap — but before it spreads out of control. What we really need, experts like Lloyd-Smith and Rosenberg say, is better surveillance in human communities — especially in ones that frequently come into contact with wildlife.
That means setting up sentinel clinics in viral hot spot regions that can screen sick patients for the usual infectious suspects. Central laboratory facilities could hunt for less typical, or completely unknown, infections, if those initial screens come up negative. Rosenberg is currently piloting such a system in Uganda.
The World Health Organization has launched a project called the R&D Blueprint, to spur development of countermeasures for the diseases the agency believes pose the most critical risk, including Crimean-Congo hemorrhagic fever.
Preventing pandemics
Using mathematical modeling approaches, scientists have estimated there may be about 1.3 million undiscovered viruses in the world — “plus or minus,” Carroll said. Of those, about a half million may be zoonotic — viruses that can jump from an animal species to infect and spread among people, Mazet said.
And a pilot project that has been underway for the past seven years — called PREDICT — has discovered about 1,000 new viruses. The Global Virome Project, a nascent effort being driven by a community of interested scientists, would be an extension of this type of work. The approach, they believe, may be more critical now than ever.
Planners of the Global Virome Project have estimated it would cost about $3.4 billion to locate and gather at least preliminary information on 99 percent of those unknown viral threats. (The other 1 percent are so rare that setting out to find them too could nearly double the cost of the effort; no one seems to be pushing for that at this point.)
Peter Daszak, an epidemiologist with the research and conservation nonprofit EcoHealth Alliance, wants to find these viruses before they make anyone sick. “If we allow these viruses to get into people, it’s already too late,” he says. To do that, he and his team hunted through the scientific literature to create a database of nearly 600 viruses and the more than 750 mammals they infect. Then, the researchers looked for patterns that could help them understand what makes an animal virus more likely to infect humans. Their research was published this week in the journal Nature.
Scientists are racing to find ways to predict which infectious disease might emerge and threaten humans next, which could give us more time to implement prevention strategy. Many strategies are being implemented , some are hunting for viruses in animals, which are likely to infect people.
DARPA’s PREEMPT aims to predict and Prevent Viral Disease Outbreaks
With U.S. military forces deploying throughout the world, the Defense Department’s PREEMPT program is designed to preserve military readiness by protecting troops from infectious diseases. Instead of treating people, PREEMPT focuses on animal reservoirs and insect vectors where viral pathogens originate.
Numerous trends including increased interactions between human, animal, and insect populations due to globalization, densification of livestock production, and rising human encroachment into animal habitats have increased the threat of novel pathogens in regions where troops, humanitarian workers, and peacekeepers tend to deploy.
Despite global biosurveillance efforts, viral outbreaks continue to outpace medical preparedness. That means that in volunteering to be the first ones into harm’s way, our Service members can quite literally be among the first people exposed to emerging infectious diseases,” said Jim Gimlett, the PREEMPT program manager. “DARPA wants to reorient preparedness efforts to make them more proactive, so that instead of only modeling the trajectory of an epidemic as it spreads from human to human, we contain and suppress diseases in the animal species in which they originate before they can make a jump into people.”
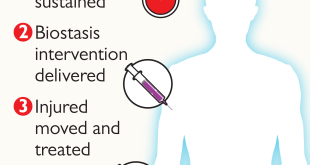
PREEMPT will have two technical thrusts, including an assessment of the likelihood that a selected animal-based virus, or multiple related viruses, will jump to humans in a targeted geographic area; and methods for suppressing the virus either in a typical animal host or a potential vector for transmission to humans, such as livestock or mosquitos.
The Program requires development of multiscale models and test beds to quantify the imminent emergence and reemergence of human pathogens; and development of new, scalable approaches to preventing pathogen spillover and transmission from animals and vectors into humans. The solicitation suggest that gene editing, antibodies, defective interfering particles, and vaccination may ultimately present viable solutions. However, the solicitation also strongly encourages offerors to identify novel approaches. In addition, the solicitation encourages offerors to pursue approaches that do not require individual treatment of animals and only activate in the presence of a targeted virus.
Understanding how viruses evolve within a species will be a core area of research. That evolutionary process contains natural bottlenecks that could be exploited to impede dangerous mutations. PREEMPT will seek to identify these opportunities for intervention by modeling the factors that enable species jump. Researchers on the program will be required to conduct field surveillance of animal and insect species in high-risk areas around the world; generate data in lab testing and sequence viruses as they evolve; analyze the jump risk by weighing factors such as past known jump events, ecology, seasonal variants, and geospatial data; and, finally, validate models using simulated natural environments.
New proactive interventions will center on methods for disarming a virus before it can make a jump across species. PREEMPT aims to prevent transmission of virus from a reservoir species direct to humans, from a reservoir species to traditional vectors, such as mosquitos, that spread disease, and from a reservoir species to a species intermediate to humans—for example, from bats to pigs.
Successful interventions will be tailored to anticipated threats. For instance, if a single mutation is identified by models as high risk, an intervention might seek to prevent its entry into a new species by removing that specific mutation from the reservoir. Alternatively, if multiple potential threats are identified, an intervention could involve treating the entire animal reservoir to reduce viral load using tools such as anti-virals, vaccines, and interfering particles. Other forms of intervention might involve new approaches to suppressing the transmission of specific viruses by insect vectors. In all cases, researchers will need to develop scalable methods that can be readily deployed even in remote locations.
During the planned 3.5-year PREEMPT program, DARPA aims to identify signatures of viral fitness and the potential for spillover from one species to another; develop risk classifiers and predict pathways of viral adaptation; and test initial intervention approaches. By the end of the program, DARPA seeks to demonstrate in controlled laboratory conditions the suppression of viral jump to a new species.“If we are able to predict how viruses might mutate and spread, and take steps to prevent those mutations from impacting humans, then we’ll vastly diminish the possibility of future viral pandemics,” said Gimlett.
Although PREEMPT is a fundamental research program, DARPA is aware of biosafety and biosecurity sensitivities that could arise. The agency will work with external bioethics advisors to ensure efforts funded by the program adhere to regulations and ethical best practices. Proposers will also be required to address potential ethical, legal, and societal implications of the research.
PREEMPT Awards
The PREEMPT research team, led by the One Health Institute at the UC-Davis School of Veterinary Medicine and the Center for Comparative Medicine at the UC-Davis School of Medicine and veterinary school, will concentrate efforts on the Lassa and Ebola viruses. Both zoonotic viruses are seen as significant biological threats to deployed military personnel, local communities in West and Central Africa, and global health security.
The first phase of the project is underway in Sierra Leone. Field teams will collect and test samples from Mastomys rats, a widespread local rodent and known reservoir for Lassa virus.The team works closely with the Sierra Leone government, University of Makeni, Njala University, and community partners, leveraging relationships established over the past five years through the U.S. Agency for International Development–funded Predict project, also headquartered at the UC-Davis One Health Institute.
Researchers will integrate data from the field studies, along with viral testing and probability models, to predict the real-time risk for the emergence of Lassa virus and spillover into people.”PREEMPT takes a deep dive into Lassa virus and its ecology,” said Dr. Brian Bird, co-principal investigator of the PREEMPT project and global lead of Predict-Sierra Leone, in the press release. “We want to understand why one particular variant of the virus spills over into people versus another.”
In the program’s second phase, researchers will design and test a novel vaccine in collaboration with The Vaccine Group and the Leibniz Institute for Experimental Virology. “A vaccine designed for broad uptake within a specific animal community could be a game changer,” said Peter Barry, PhD, co-principal investigator and professor emeritus with UC-Davis Center for Comparative Medicine, in the press release. “If we can disrupt the spread of a virus within an animal community, we will help to eliminate the threat of animal diseases ultimately spilling over into humans.”
The One Health Institute has been integral in global surveillance of zoonotic disease and capacity building through its leadership of Predict. In 2018, the Predict team announced the discoveries of a new species of ebolavirus and a closely related cousin, Marburg virus, in bats in Sierra Leone prior to those viruses ever being detected in a sick human or animal.
The PREEMPT team’s plan to use cytomegalovirus, a common virus, to vaccinate animals against other viruses, such as Lassa virus and Ebola virus, is a direct result of work initiated by Dr. Barry to develop a nonhuman primate model of human cytomegalovirus.
“This type of collaboration across disciplines made possible through this DARPA cooperative agreement is how we’ll get in front of the unpredictable nature of zoonotic diseases,” said Dr. Michael Lairmore, dean of the UC-Davis School of Veterinary Medicine, in the press release. “PREEMPT exemplifies the level of innovation that’s possible using a One Health approach, and it will protect lives on a global scale.”
Cary Institute disease ecologist Dr. Barbara Han’s research program at the intersection of ecology, computing, and global public health, is developing tools to predict and preempt disease outbreaks. Dr. Han is harnessing the power of big data and machine learning to create maps of regions that are hotspots for disease spillover. By identifying animal species that are likely to harbor pathogens and pinpointing where their populations intersect with people, her work can guide disease surveillance and protect public health. Han’s projects with IBM and DARPA, are investigating how Climate change and urbanization influence zoonotic disease transmission, what traits make animals risky neighbors, and the critical role of basic science in making accurate predictions to safeguard public health.
Abcellera is working to identify antibodies that can neutralize the virus and potentially block its transmission. Since 2018, under the DARPA Pandemic Prevention Platform (P3) program, AbCellera has been developing a “technology platform for pandemic response capable of developing field-ready medical countermeasures within 60 days of isolation of an unknown viral pathogen.” Abcellera told us that a key aspect of this work is to “deliver an antibody countermeasure as a nucleic acid vector instead of recombinant purified protein.” In other words, the patient’s own cells will manufacture the therapeutic instead of it being manufactured in a lab outside of the patient. This is a relatively new way to deliver the drug — or more precisely, the genes to make the drug.
References and resources also include:
https://medicalveritas.org/darpa-and-coronavirus-western-hands-in-plague/
 International Defense Security & Technology Your trusted Source for News, Research and Analysis
International Defense Security & Technology Your trusted Source for News, Research and Analysis