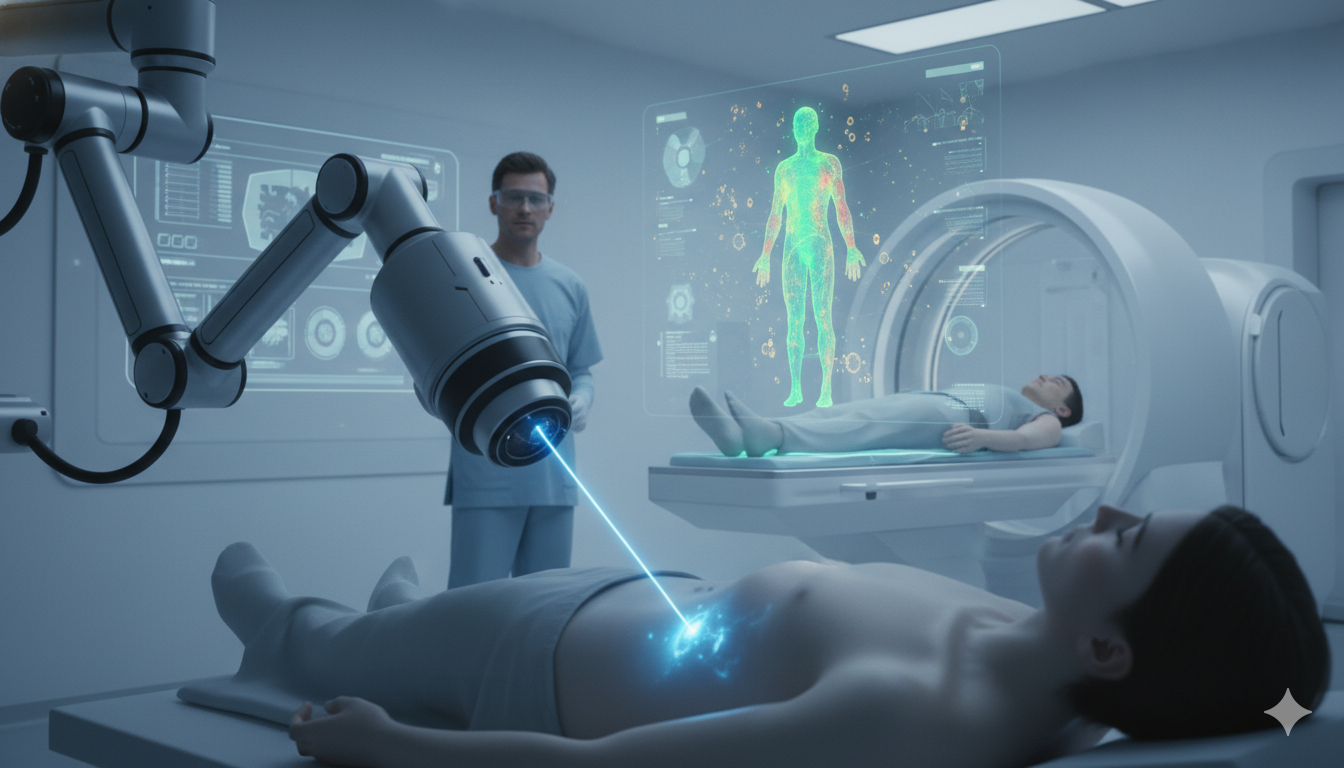
The human body operates through complex electrochemical and optical signaling networks, where photons play a critical role in cellular communication, neural transmission, and metabolic regulation. Advances in photonic engineering—particularly lithium niobate photonic chips, precision lasers, and optical biosensors—are enabling clinicians to observe, diagnose, and treat disease with unprecedented sensitivity and specificity. These technologies allow detection…