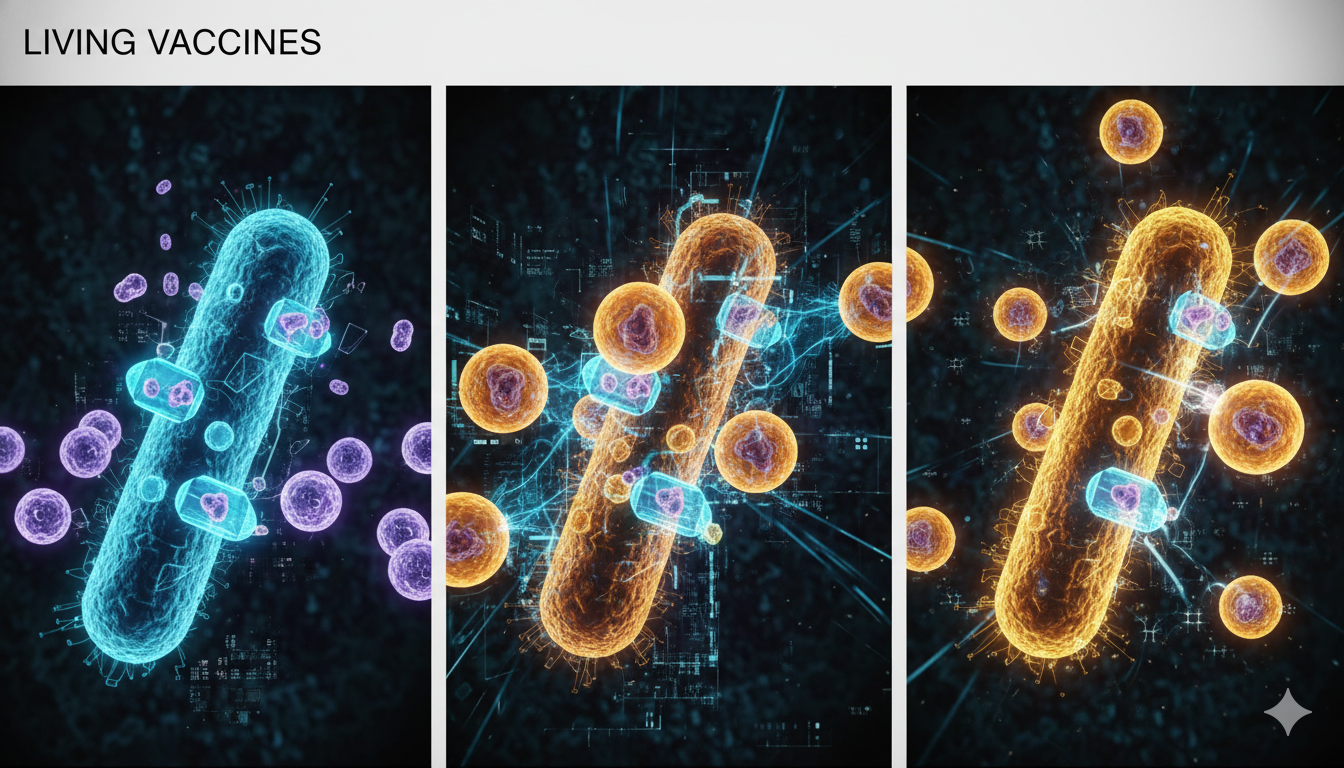
Synthetic biology is transforming bacteria into living cancer therapies—capable of infiltrating tumors, activating immune responses, and reshaping the future of precision oncology. For decades, cancer treatment has relied on the familiar triad of surgery, chemotherapy, and radiation. More recently, immunotherapy has offered new hope, especially with checkpoint inhibitors and CAR-T cells reshaping treatment landscapes. Immunotherapy…